COMMUNICATING ABOUT VAPING
A rebuttal to the “Science has Marched On” report by Physicians for a Smoke-Free Canada
Dr. John Oyston - Dr. Chris Lalonde - Dr. Mark Tyndall - April 13th, 2022
The 4.2 million Canadians who smoke cigarettes need accurate information about the alternatives that are available to them if they want to avoid the serious health risks of continuing to smoke tobacco.
Many people who smoke have already tried and failed to quit, either by going “cold turkey” or by using medical nicotine replacement therapy (NRT) such as patches and gum, but their dependency on nicotine leads to withdrawal symptoms and cravings that cause them to relapse into smoking.
If people were properly informed about alternative sources of nicotine, such as vape (“e-cigarettes”), heat-not-burn devices and oral tobacco such as snus, many would choose an option that provided the nicotine while greatly reducing the harmful health effects of smoking.
Accurate information about nicotine and vaping is hard to find. Media outlets tend to emphasize extremely rare risks, like exploding vapes, rather than smokers who have quietly switched to vaping and are now healthier. Unfortunately, many medical organizations and public health groups have adopted a prohibitionist stance against vaping and against nicotine.
Misinformation and lack of public health leadership not only discourages people from transitioning to life-saving alternatives but makes national targets for smoking reductions unattainable.
Physicians for A Smoke Free Canada (PSFC) recently published a report entitled “Science has marched on: it’s time to update the advice to Canadians” (PSFC Staff – February 14, 2022). We can totally embrace the title of the report but reject the contents and messaging. They argue that the latest research on vaping should lead Health Canada to warn young people that “Smoking kills, and vaping almost certainly kills too” and to tell smokers trying to quit that “Using e-cigarettes will likely decrease the chances of success and will increase health risks in comparison with approved smoking cessation aids.” We strongly believe that this is the wrong message and is not supported by the science. If left unchallenged, it will prevent smokers from switching to less harmful sources of nicotine, resulting in literally thousands of deaths and greater profits for the tobacco industry. It will also encourage all levels of government to make vaping less attractive to both smokers and non-smokers, and therefore less effective as a way to quit smoking, by imposing artificially low nicotine levels, flavour bans, high taxes, and restricted access.
Who are Physicians for a Smoke-Free Canada?
Physicians for a Smoke-Free Canada gives the impression of being an independent grassroots organization representing Canadian physicians who are opposed to smoking. However, for the years 2016-2020 only 6% of their income come came from donations and 65% came from government grants. They do not run any smoking cessation clinics or other charitable programs; they just take government money and then use those funds to lobby the government.
PSFC is made up of a board of seven physicians and two staff. All its recent publications are attributed to “PSC Staff.” This means Cynthia Callard and Neill Collishaw, who are not physicians. They have written extensively on tobacco control issues for many decades. From their publications, it is not clear what degrees they hold, and it seems as though they have no university affiliation.
Their “@DocsVsTobacco” Twitter tagline says: “After 34 years, still working to reduce the toll of nicotine addiction in Canada!” This is curious, as nicotine addiction is not lethal, but cigarettes kill 48,000 Canadians every year. Nicotine has medicinal uses and is recognized as an essential medication by the WHO.
In a November 2021 tweet, they stated:
Our recommendations include 2 new policy directions:
1. Prevent addiction. Adopt as a policy goal the end of commercial nicotine and tobacco use.
2. Reform supply. De-commercialize harm reduction, cap production, reform retail.
They want nicotine prohibition and to prevent the legal sale of less harmful nicotine products such as vape and snus.
One of the directors of PSFC, Dr. Andrew Pipe, runs a smoking cessation conference that depends on funding from Pfizer and Johnson & Johnson. He bans people who own vape shops from attending and learning about smoking cessation, on the basis that they have a “conflict of interest with the content”.
(PSFC was shown a draft of this statement and were given the opportunity to fact check it. They declined.)
PSFC correctly states that there have been over 4,000 scientific articles published about vaping in 2020 and 2021. Science is about the quality of the data, not the number of publications, and many of these articles are fundamentally flawed. The composition of e-juices and of vape have not changed significantly in the years since Public Health England re-affirmed that vaping is 95% safer than smoking. People who are opposed to vaping are still referring to popcorn lung (a theoretical risk of vaping that has never occurred in vapers) and EVALI (that was caused by contamination of illicit THC products) as examples of the harm caused by vaping. This deception not only creates confusion in the minds of the public but also undermines trust in public health.
Modern electronic cigarettes were invented by Hon Lik, a Chinese pharmacist, in 2003 and have been commonly used for over a decade. It is estimated that they are used by about 68 million people globally. Although we still lack rigorous longitudinal studies to determine the long-term safety of vaping, there is currently no evidence to suggest unexpected adverse health effects. At this point in time, we can be confident that when compared with smoking cigarettes, the long-term health outcomes of people who vape will be much less disease and death.
It is not unusual for health care to progress without evidence of long-term effects. If a new medication, operation or surgical implant is developed, it will gain approval and widespread usage without waiting for a ten-year follow up to prove its safety and effectiveness. For example, the Covid vaccination was first used in December 2020 and by March 2022, with only 16 months of follow-up data, it had been given to over 5 billion people.
The issues raised by the PSFC report
While we disagree with most of the content, conclusions, and recommendations of the PSFC report, it does raise important issues that have influenced public perceptions and government policies around vaping both in Canada and globally. These will be discussed in the next seven parts of this report:
1) Are more young people using nicotine?
2) Is vaping a “gateway” to tobacco use or a diversion from it?
3) Is “dual use” of cigarettes and vape “common and harmful?
4) Are e-cigarettes effective as a way to quit smoking?
5) What are the harmful effects of vaping and how do they compare to smoking?
6) What are other governments doing about vaping and are there examples for Canada to follow?
7) What should Canadians be told about vaping?
Part 1: Are more young people using nicotine?
Dr. Chris Lalonde
PSFC states that “E-cigarettes have increased the number of young nicotine users in some countries”
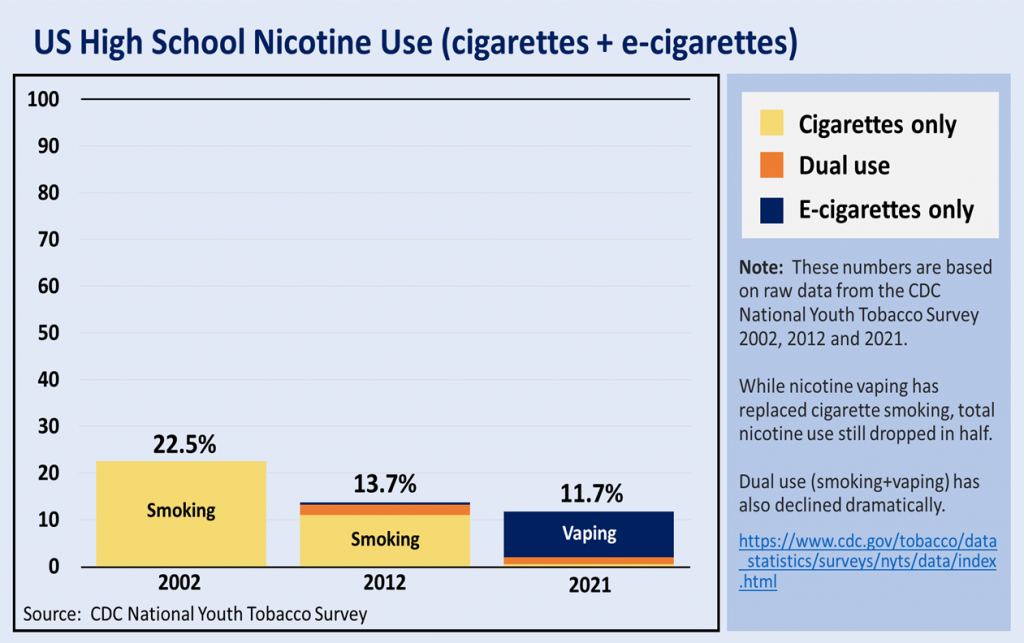
Given the name of the organization, one would think that the goal of Physicians for a Smoke-Free Canada is to remove tobacco smoke rather than nicotine. Tobacco smoke is uniquely toxic, nicotine is not. We have nicotine products that are approved for use in Canada (patches, gums, inhalers, etc.) and these products are often subsidized by provincial health authorities. Their concern about the “number of young nicotine users” means that they are mixing apples and oranges, lumping together young people who smoke with young people who vape, as if they were similar, ignoring the evidence that smoking is many times much more dangerous than vaping. But, in fact, the most recent data shows that in both the USA and in Canada, smoking, vaping and “total nicotine use” are all decreasing.
In the USA, youth vaping rates fell by 62%, from 22.4% to 9.8%, between 2019 and 2021. Youth cigarette smoking rates in the USA are now at the lowest level ever recorded at 1.9%. The total number of “nicotine users” has halved.


According to Statistics Canada the daily or occasional youth smoking rate was 1.8% in 2020—a 72% decrease from the previous year. The daily smoking was described as “unreportable due to small sample size.”
Youth vaping in Canada is also declining slightly. Data from Statistics Canada reveal that in 2019, 15% of youth 15-19 had vaped at least once in the past 30 days, and 26% of these youth were current or former smokers. This vaping prevalence is now 14%. The data does not support PSFC’s contention that “nicotine use” rates are rising in the USA or Canada. More importantly, those youth who are using nicotine, are choosing a less harmful nicotine source, by vaping instead of smoking. This should be considered a triumph for public health.
PSFC erroneously states that both smoking and vaping are increasing in New Zealand. According to Action on Smoking and Health, the youth daily smoking rate is continuing to fall and is now a record low 1.3%. Youth vaping rates are increasing, partly due to the government’s Quit Strong campaign aimed at persuading young smokers to switch to vaping.
Conclusions
We can lament the use of nicotine by young persons, but we need to ask: would we rather they smoked cigarettes, or wore a patch, or chewed some nicotine gum, or vaped? Smoking is declining and it is not all clear that nicotine use (absent burning tobacco leaves) is actually a threat to health.
Multiple studies show that former smokers who take up vaping reduce rather than increase their nicotine consumption over time. This runs counter to the addiction narrative. Studies that claim nicotine use damages adolescent brains are based entirely on studies of rodents. There is not a single study of humans that supports that claim. One need only ask where are all the ‘brain damaged’ adults who started smoking as teens in the 1960s?
Reports of associations between smoking/vaping and teen anxiety, depression, and other mental health issues seem to miss the point. There is simply no evidence that smoking or vaping cause these conditions. Rather it is abundantly clear that persons living with these conditions are using nicotine to improve concentration and cope with daily stress. We can stigmatize these young people (see the shameful Depression Stick campaign from Truth Initiative), or we can collectively and more seriously think about the daily circumstances that these young people endure.
Rather than fretting about vaping or youth smoking, perhaps we (as parents, educators, politicians) should consider the things that truly put young lives in danger. According to the USA Centers for Disease Control, here are some more important public health issues to worry about:
• 39% text/email while driving
• 30% drink alcohol
• 20% use marijuana
• 17% ride with a driver who had been drinking
• 17% considered suicide in the past year
• 16% carry a weapon
• 14% binge drink
• 13% drive after marijuana use
Part 2: Is vaping a “gateway” to tobacco use or a diversion from it?
Dr. Chris Lalonde
PSFC states that “Young people who use e-cigarettes are more likely to smoke conventional cigarettes.”
This is the dreaded “gateway effect”—the notion that puffing on an e-cigarette will lead to a life-long addiction to smoking cigarettes. If there were any truth to the gateway hypothesis, then smoking rates should be increasing. But they aren’t. Youth smoking rates decreasing in the USA and Canada.
“Gateway Theory”, “Common Liability” and “Diversion Theory”
There is abundant evidence that youth who experiment with vaping also experiment with smoking. Initially there was a concern that vaping might be a gateway to smoking, just as “soft drugs” may be a gateway to “hard drugs”. However, both cigarettes and vape provide similar amounts of the desired substance, nicotine. There is no need for a vaper to switch to smoking when if they can just switch to a vape juice with a higher nicotine concentration. Vaping is cheaper, safer, more convenient and trendier than smoking. The alternative “Common Liability” theory suggests that some teens are predisposed to be adventurous and to experiment with forbidden things, and they will try both smoking and vaping. The data now also supports the “Diversion Theory” that vaping is diverting teens who would otherwise have smoked into using a less harmful product.

According to the “Gateway Theory” the increase in teen vaping that started in 2013 should have resulted in an increase in teen smoking in subsequent years. In fact, the decline in smoking rates became steeper as teen vaping became more popular.
PSFC cite an article by Creamer at al. (2020) as supporting the gateway hypothesis. The question of whether youth e-cigarette use can lead to smoking initiation simply cannot be answered using cross-sectional data. Cross-sectional studies provide a single ‘snap-shot’ in time—they do not follow individuals over time and cannot be used to establish whether there is a causal relationship between observations of two variables. Even Creamer et al. acknowledge this. In discussing whether the results of their own current and previous studies they state: “these findings may suggest that most current e-cigarette users may have been unlikely to have smoked cigarettes” and note that “due to the cross-sectional nature of NYTS data, this hypothesis cannot be fully tested using this data source.”
To support the claim that “adolescents who use e-cigarettes are at least three times more likely to take up smoking than non-users of e-cigarettes” PSFC cite the Yoong et al. (2021), meta-analysis. This is odd, since Yoong et al., conclude that: “Among current ENDS/ENNDS users, there was a significant association with ever, but not current cigarette use at follow up”.
It’s not clear why anyone should be concerned about “ever use” rather than “current use” (even if that might be a single puff in the last 30 days).
PSFC also cite Staff et al., 2021 noting that it is a longitudinal rather than cross-sectional study. “Among youth who had not smoked tobacco by age 14… teenagers who used e-cigarettes by age 14 compared with non-e-cigarette users, had… nearly triple the odds of being a frequent tobacco smoker at age 17… among youth who had not used e-cigarettes by age 14… teenagers who had smoked tobacco cigarettes by age 14 had … three times higher odds of frequently using e-cigarettes at age 17.” Three times higher for both groups. This really seems like a ‘pick your poison’ moment. Which would you rather have youth initiate: cigarette smoking or e-cigarette use?
It has never been clear just how long should we wait for evidence of a gateway to youth smoking. Less than two young persons in 100 are daily smokers in Canada. It seems that youth are done with smoking.
Recommendations
Perhaps we should shift our attention to the millions of adult Canadians who still smoke cigarettes. Can we help them understand that nicotine doesn’t cause cancer? Can we help them access e-cigarettes with nicotine levels high enough to replace the cigarettes they currently smoke? Can we make e-cigarettes more affordable, more accessible, and more attractive than tobacco? Yes, we can and we should. And we can do all of that while restricting youth access. It’s not hard. We already have laws against selling e-cigarettes, alcohol, marijuana to youth. Just enforce them!
Part 3: Is dual use of cigarettes and vape “common and harmful”?
Dr. Mark Tyndall
Dual use (concurrent vaping and cigarette smoking) has become a major focus for those opposed to vaping. Opponents claim that there is little to be gained from vaping if a person continues to smoke cigarettes, and point to surveys that consistently show that a significant proportion of people who vape continue to smoke. The PSFC claims around dual use are based on the Health Canada statement about health improvements for those who “completely replace cigarette smoking with vaping.”

The report then shows a graph from two on-line surveys that show that a proportion of people who report using e-cigarettes in the past month also report smoking. While some people have certainly continued with dual use, these surveys are cross-sectional and are not able to differentiate between the people who are in transition to exclusive vaping versus those who will continue to smoke and vape. In fact, it would be expected that most people who initiate vaping will start by slowly replacing some of their cigarettes as they try different delivery systems, nicotine content and flavours.
From an individual perspective, the goal should be the total elimination of cigarette smoking. It has been shown that the risk of cardiovascular disease due to smoking does not follow a linear dose-response curve and that simply swapping out a few cigarettes with vaping will not significantly reduce the long-term risk. However, on the road to quitting cigarettes, any reduction should be considered a positive step. Historically, the message of tobacco control advocates and the medical profession has been to reduce the number of cigarettes smoked with the aim of quitting. It is still better to consume half a pack of cigarettes per day than a full pack. As with any behavioral modification, the process of a gradual change is ultimately much more successful than a “cold-turkey” approach. Ironically, this stepwise introduction is exactly how we promote nicotine replacement therapy (NRT) using patches and gums. We would never tell someone to stop NRT because they are smoking the occasional cigarette.
What is most problematic with the current messaging is that it actually contributes to the persistence of dual use. If people are told that dual use is dangerous then they will be less likely to try vaping in the first place. The PSFC statement “that using both e-cigarettes and conventional cigarettes is likely more harmful than only smoking or only vaping” is not only grossly inaccurate but is very confusing to people trying to reduce their health risks by vaping. It would be like saying that using both NRT and conventional cigarettes is more harmful than smoking alone. With clear and accurate information, it is much more likely that dual users will fully transition to vaping.
There are three references used in the PSFC report to support their claims around dual use. The first reference is a large cross-sectional study (Health eHeart) that looked at self-reported cigarette and e-cigarette use. They found that dual users reported more severe respiratory symptoms compared with the vaping-only and smoking-only groups. For smokers with more severe respiratory symptoms, it is expected that they would be more likely to try vaping as a way to reduce their respiratory limitations. Therefore, it is predictable that in a cross-sectional analysis that dual users would report worse respiratory symptoms compared with the only smoking group. The other major finding of the paper was that exposure to combustible cigarettes was the same among those who reported smoking only and those who reported dual use. This means that the people in the survey were not able to reduce their cigarette use which is clearly not the aim of vaping. The focus should be on helping people to reduce/eliminate cigarette exposure. It is an erroneous conclusion that dual use is riskier than smoking.
The second reference was from the infamous Stanton Glantz group at the University of California that was published in 2018. They showed a high risk of myocardial infarction associated with e-cigarette use even when adjusted for cigarette use. This paper is weirdly similar to the 2019 publication in the Journal of the American Heart Association (JAHA), where identical claims were made. The JAHA paper was one of the most damaging articles ever published about vaping and received widespread media attention. However, when it was pointed out that the study included participants who experienced a cardiovascular event prior to initiating e-cigarettes, the Journal asked for a re-analysis. When it was clear that the authors could not provide this, the paper was retracted by the Journal. The retraction of an article after publication is very unusual in academic publishing and usually represents academic misconduct and not simply an oversight in the analysis. Anyone involved in tobacco control must know about the controversy surrounding the false claims of the Stanton Glantz group and it undermines the credibility of the entire PSFC document.
The third reference, by Okunna, looked at mental and behavioral health risks among dual users, exclusive cigarette users and non-users from a cross-sectional survey. The author found that dual users reported more days of poor mental health, as well as more cannabis, alcohol and smokeless tobacco use. They concluded that ” these findings may be indicative of increased health risks associated with dual use, compared with the exclusive use of tobacco cigarettes”. Dual users may indeed use more substances and have poorer mental health outcomes, but this in no way points to causation or shows that exclusive cigarette use should be encouraged over dual use.
Conclusions
We can all agree that the goal should be to phase out cigarettes and eliminate exposure to the deadly chemicals released through combustion. The focus now should be how we best help people to fully move away from cigarettes. However, taking a position that dual use is unhelpful or even dangerous is disingenuous and not supported by the scientific evidence provided.
Part 4: Are e-cigarettes effective as a way to quit smoking?
Dr. Mark Tyndall
The PSFC claim that e-cigarettes are not an effective smoking cessation tool is dishonest and most vaping opponents have distanced themselves from this position. Martin Dockrell from Public Health England said it best, “the claim that e-cigs can’t help people quit smoking is now so plainly false that anybody making it not only discredits themselves, but worse still, undermines public confidence in science.”
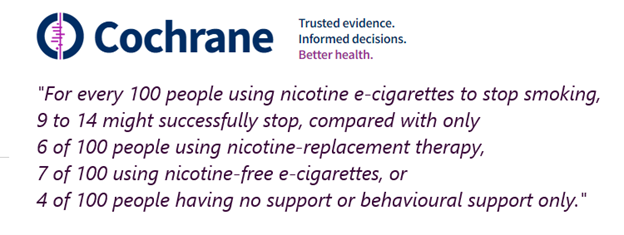
Clinical trials and systematic reviews show that vaping is currently the most widely used smoking cessation intervention and is superior to NRT and other cessation interventions. The PSFC report tries to focus on the use of e-cigarettes as “consumer products” and they argue that when vaping is used in real-world situations it is not effective as a cessation tool. They reference a Cochrane review [letter Q in the report] to support this claim. What they do not mention is that the Cochrane review concludes that nicotine-containing e-cigarettes are superior to NRT, non-nicotine-containing e-cigarettes and behavioural interventions in helping people quit cigarettes.
The PSFC report fails to recognize that vaping is driven primarily by people who smoke cigarettes and have purchased their vaping products in vape shops, online websites, and through a variety of commercial outlets. There are an estimated one million Canadians who have partially or entirely switched from cigarettes to vaping. While there has been a concerted effort to make commercial cigarettes less attractive (i.e., graphic images on packaging, plain packaging, restrictive advertising regulations, etc.) and less accessible (i.e., high taxes, restricted product displays, etc.) they are nonetheless readily available as a consumer product in Canada. Government restrictions have been designed to make cigarettes less accessible to younger people and have likely reduced smoking initiation, but it is unclear what impact these measures have had on helping cigarette smokers to quit. It is certain that these policies have contributed to poverty by disproportionately taxing the poor, the creation of a robust illicit cigarette market, and more shame and isolation for those who smoke.
The importance of offering access to vaping through commercial outlets is further supported by the community of vaping advocates who have successfully transitioned to vaping. A recent study showed that among 40 heavy smokers who had switched to vaping, 17 had switched “accidentally” after being offered a vaping device by a friend or on a whim. After initial use, they discovered that they liked the experience and ultimately gave up smoking. While this is a small study, it reflects the real-life experience of many people who vape and makes it clear that people need a wide range of opportunities to access vaping products. For example, regulations that would limit access to medical prescription models only would fall short.
It is illogical and reckless to promote policies that would restrict or even ban the sale of vaping products in places where cigarettes are available. There is really no precedent in public health where a much safer medicine or medical device or procedure is introduced and then is heavily restricted or prohibited, while the deadly medicine/device/procedure is allowed to continue. This is exactly what is happening with e-cigarettes/vaping and all safer nicotine delivery systems.
The PSFC report carefully hand-picked published studies that appear to support the claim that e-cigarettes are not effective for smoking cessation. One of the main references is a study from Richard Wang and Stanton Glantz who conducted a large meta-analysis of both observational studies and randomized clinical trials that looked at e-cigarettes and smoking cessation. Oddly, they combined people who had fully transitioned to vaping with those who had used e-cigarettes but continued to smoke and concluded that smoking cessation was not associated with vaping. However, when they looked at people who had completely transitioned to vaping, the people of interest, more people had quit cigarettes.
A paper by Chen R. et.al. came from a large survey study called PATH that concluded that using e-cigarettes was not effective for quitting following analysis of responses collected between 2017 and 2019. They reported that people who used e-cigarettes as an aid to quitting were only half as likely to succeed as people who did not report using any cessation related aids. Interestingly, they reported that 18% of respondents were able to quit with no cessation aids at all which is far higher than other studies. These findings remain a distant outlier when compared with the scientific literature. In fact, the next study cited in the report by McDermott MS et. al. showed the opposite results in a survey from the United Kingdom. People who used e-cigarettes were much more likely to successfully quit cigarettes. They did find that non-daily or occasional e-cigarette use was not associated with smoking cessation. This is not an argument against e-cigarette use but rather shows that a full transition to vaping is required for success.
One of the most curious references cited to support the argument that e-cigarettes are not effective was by Kasza KA et.al. This study is often cited by vaping advocates to support the use of e-cigarettes for smoking cessation. In this study, the authors looked at smokers who were not planning to quit but had tried e-cigarettes for other reasons. They found that those who began to use e-cigarettes daily were eight times more likely to stop smoking than those who didn’t use e-cigarettes at all. As in other studies, non-daily e-cigarette use was not associated with smoking cessation. This observation also emphasizes the need to educate and support smokers to fully transition to vaping.
The study cited by Zhang et.al. was a meta-analysis of four published systemic reviews and included five RCTs and 24 cohort studies. The RCT findings showed unequivocal benefits of e-cigarettes for smoking cessation, while the cohort studies were less consistent with some of the studies included in the analysis showing no benefit. The intensity of e-cigarette use was an important predictor of success, with more consistent use being associated with quitting. Even in this paper, the overall conclusions were that “e-cigarettes appear to be potentially effective for smoking cessation”.
A study cited by Barufaldi et.al. found that people who were long-term former smokers who started to vape were more likely to relapse back to cigarettes. As the authors described in the limitations section of the paper, the meta-analysis only included six studies with wide heterogeneity. There is no question that long-term smokers who quit by vaping are at risk of relapse, and that some may resume vaping to prevent a return to cigarettes. That in no way shows that vaping contributed to a relapse to cigarette smoking. In fact, for many former smokers, vaping would be a way to prevent such a relapse from happening.
Conclusions
In Canada, we should be well past the stage where we need to convince people that vaping is an effective way to quit smoking. It has worked for literally tens of millions of people worldwide despite the misinformation that continues to be perpetuated by anti-tobacco groups such as PSFC, who doggedly cling to abstinence only ideologies.
While more longitudinal studies should be conducted, it is time to promote vaping as a first line intervention for people who want to stop smoking cigarettes. Some of the inconsistent results found in observational studies are almost certainly due to the misinformation that smokers must wade through as they decide whether to try and/or continue to vape.
To rapidly scale up vaping as a life-saving public health strategy, vaping must be made more accessible, more attractive and cheaper than cigarettes. This can only happen by stopping the spread of misinformation, especially by government funded lobbying groups.
Part 5: What are the harmful effects of vaping and how do they compare to smoking?
Dr. John Oyston
PFSC says that “E-cigarettes cause damage to respiratory and circulatory systems.” This is undoubtedly true. E-cigarettes are not harmless. Vaping exposes people to levels of pollutants similar to living in a big city.
However, cigarette smoking is VERY dangerous, as over half of all long-term tobacco smokers will eventually die as a result of the toxic effect of inhaling burnt tobacco leaves. The important questions are “How does the harm from vaping compare to the harm from smoking?” and “Are there health benefits when smokers switch to vaping?”
Cigarettes cause harm in three main ways. They cause lung and other cancers, they damage the cardiovascular system, resulting in many conditions including heart attacks, strokes and peripheral vascular disease and they damage the respiratory tract, mainly causing COPD. These risks need to be considered separately.
PSFC calls “Cardiorespiratory and Immunologic Effects of Electronic Cigarettes” a “useful summary”, but in fact it makes no comparisons between smoking and vaping. The authors make the curious statement “if e-cigarettes are half as harmful as combustible cigarettes, but are used twice as much, there would be little harm reduction by using e-cigarettes over combustible cigarettes.” They also state that “the national outbreak of EVALI brought to fore not only the risk of inhaling mixtures of unknown constituents, but also the risk that may be associated with the use of e-cigarettes”. This is a strong argument for ensuring a regulated, legal supply of vape to avoid creating an illicit market like the homemade THC products that led to EVALI.
There have been many misleading studies about the health effects of vaping. Some researchers claimed to find a causal association while not supporting such findings with meaningful data: their discussions and conclusions are therefore misleading,
Health effects of vaping
Side effects
In an internet survey, 38.9% of 19,414 vapers reported a dry mouth or sore throat. Other side effects included cough (12.8%) headache (11.1%), dizziness (5.1%) and gingivitis (13.1%).
Cancer risks
The cancer risk from vaping is relatively easy to assess, as research laboratories are able to measure the carcinogenicity of a wide-range of toxins. Based on chemical analysis of vape, the lifetime risk of cancer has been calculated to be 0.4% of the risk from smoking. Another review and meta-analysis reported that smoking was over 400 times more likely to cause cancer than vaping.
Cardiovascular Risk
Comparative risks of cardiovascular disease and lung disease have not been quantified but are estimated to be substantially below the risks of smoking. In the absence of direct comparisons between the effects of smoking and vaping in humans many people rely on animal studies or studies that look at the harm from vaping without making a valid comparison with smoking.
One study, by Prof Stan Glantz, had to be retracted. He claimed that vaping caused heart attacks, but on review of the data the majority of the 38 patients in the study who had heart attacks suffered them before they started vaping.
In a review of the health impact of electronic nicotine delivery systems (ENDS), the authors concluded that “Our review found that ENDS product use has not been shown to be causative for harmful CVD outcomes and, indeed, has been shown to be beneficial for hypertensive patients.”
An investigation into “Cardiovascular Effects of Switching From Tobacco Cigarettes to Electronic Cigarettes” showed that within a month of smokers switching to vaping their vascular function improved significantly. Specifically, there was a significant improvement in endothelial function and vascular stiffness. Flow mediated dilatation (FMD) is 7.7% in normal healthy non-smoking and non-vaping volunteers. Smokers began the study with an FMD score of 5.5%, which increased to 6.7%, (more than halfway back to normal), after only four weeks of vaping.
A study showed smokers who reduce or quit smoking by switching to e-cigarettes may lower their systolic BP in the long term. “A slight but significant decrease in systolic BP was found at week 52 (123.1 ± 13.8 mmHg) with respect to baseline (128.0 ± 15.3 mmHg, p = 0.004).”
Respiratory risk
Some people opposed to vaping pretend that the 2019 outbreak of the severe lung disease incorrectly named “EVALI” was in some way related to legal store-bought nicotine vapes. The CDC now confirms that it was due to illegal backstreet cannabis products that were deliberately contaminated with Vitamin E Acetate for commercial gain. Health Canada continues to mention the purely theoretical risk of “Popcorn Lung” as a risk of vaping, even though they admit that no vaper has ever presented with popcorn lung from vaping.
One of the few long-term studies of vaping is a five year follow up of COPD patients who switched to electronic cigarettes (ECs). The EC users reduced their mean cigarette smoking from 22.1 to 1.4 per day. COPD exacerbations halved in the EC group and did not change in the control group. Lung function measurements (FEV1 and FVC) improved in the EC users. CAT scores (a subjective COPD assessment), significantly improved in the EC group. At five years from baseline, the EC group were able to walk 46.5 m further in six minutes than the control group.
For smokers with COPD, switching to vaping is like taking a medicine that decreases exacerbations, improves lung function and enables the patient to walk further.
A study of the “Persisting Long Term Benefits of Smoking Abstinence and Reduction in Asthmatic Smokers Who Have Switched to Electronic Cigarettes” showed significant improvements in Asthma Control Questionnaire(ACQ) scores, and all lung function parameters at 12 and 24 months.
Genetic effect of vaping
PSFC noted that “Tommasi and colleagues further investigated gene dysregulation in smokers and vapers. They found that genes that control mitochondria were disrupted both by smoking and vaping.” However, they failed to note that the report shows that vaping is, in fact, 7.4 times better than smoking in terms of potential mitochondrial gene damage.
Mental Health
There is an association between impaired mental health and both smoking and vaping. The anti-vaping “Truth Initiative” organization have called vapes “Depression Sticks”. However, in an internet survey of 1,914 vapers who had switched from smoking, 32% reported a better mood, and only 3% a worse mood after switching.
Biomarkers
Levels of markers for disease decrease when smokers switch to e-cigarettes. Dai et al. reported “There was a significant reduction in urine concentrations of TSNAs, PAHs, and VOCs when users transitioned from exclusive cigarette to exclusive e-cigarette use, with a 92% decrease in NNAL.” There was also a highly significant decrease in volatile organic compounds.
Deaths
Health Canada has “acknowledged that there have been no deaths reported as a result of vaping-related illnesses in Canada.”
In the UK over a five year period there were three deaths reported as possibly being associated with vaping in a population of 2.7 million adult vapers. The UK has a reporting system for “suspected side effects and safety concerns of e-cigarettes and refill containers”. For the period between it starting in May 2016 and January 2021 there have been 231 reports, mostly of respiratory disorders. Of the three reported deaths, one was considered to be caused by “EVALI” and therefore not due to nicotine vaping. Another report also involved medications and endocarditis, so the cause of death was unclear. The third case was of a person with pulmonary fibrosis, reported by a non-medical person, years after the patient had died, and therefore too late for any investigation. For comparison, 78,000 people die from smoking every year in the UK. That means that 390,000 smokers died during the five-year period when there were three possible (but far from proven) vaping deaths.

Self-reported health status
There have been several Internet polls of vapers to assess the self-reported health effects of vaping. While the respondents are self-selected and some would dismiss these reports as “anecdotes” there are literally thousands of people who report that their health improved when they switched to vaping.
In an internet survey of 19,414 vapers, 74.5% of respondents said that their health had improved after switching to vaping. 86.4% reported better sense of smell, 86.0% better breathing and 73.5% greater endurance.
In a Twitter poll by Dr. Gardner, 93% of 616 respondents stated that their health had improved after switching to vaping. In an online survey of 941 people who had switched from smoking to vaping, 66% reported a reduced frequency of respiratory infections. 232 vapers elaborated on positive and 15 on negative experiences.
Conclusions
E-cigarettes cause minor side effects in some users. They cause measurable changes in some aspects of cardiac and respiratory function, but most studies do not make a valid comparison between vaping and smoking, and the long-term significance of these changes are unclear. Smokers should not be confused by being told that vaping can cause “EVALI” or “popcorn lung”. The lifetime risk of cancer from vaping is less than 0.5% of the risk of smoking, and this alone should be sufficient reason to encourage smokers to switch to vaping.
Nicotine vaping has caused zero deaths in Canada. In the UK there is no clear evidence that anyone has died from vaping.
For smokers who switch completely to vaping, there are measurable improvements in cardiac and respiratory function, a decrease in the level of biomarkers of disease and subjective improvements in health.
A paper entitled “Electronic cigarette use and harm reversal” concluded that ”the emerging evidence that EC use can reverse harm from tobacco smoking should be taken into consideration by regulatory authorities seeking to adopt proportional measures for the e-vapor category”.
Part 6: What are other governments doing about vaping and are there examples for Canada to follow?
Dr. John Oyston
Canada has historically been a leader in public health and tobacco control. While it may be useful to look at what other countries are doing, Canada should chart its own course. In 2016 Canada committed to a “Tobacco Endgame” target of 5% by 2035 but we never developed a strategy to achieve that goal. We will not succeed with traditional tobacco control measures alone.
Why many governments are slow to act
Government actions depend not only on what is best for public health, but also on financial considerations. They may feel the need to retain tax income and protect jobs and investments in the tobacco industry that are under threat from less harmful nicotine products.
As a result, governments take different views on tobacco harm reduction ranging from enthusiastic endorsement in the UK and New Zealand to a complete prohibition on vaping in India and snus in the European Union. It is easy for PSFC to cherry pick six examples from 195 world governments that have recently published reports sceptical of vaping, and ignore countries that are supporting vaping or other less harmful nicotine products for tobacco harm reduction.
PSFC refers, for example, to the flawed EU SCHEER report. “The SCHEER report is far from being an objective research paper. Although the judgment of relative risks is key to the harm reduction approach, the report was set up in a way that no comparison be made between vaping and smoking. This request resulted in a pointless paper, with little scientific value, completely ignorant (purposefully or not) of the concept of harm reduction. Unfortunately, some policymakers are using this report as an instrument to argue for unjustifiably harsh regulation of vaping.” – Bernd Mayer Professor of Pharmacology and Toxicology at the University of Graz, Austria, November 2021.
Governments respond to public pressure. Voters are not outraged and demanding government action about the eight million people who die from tobacco use every year. Tobacco taxes are a steady stream of income. When smokers die ten years prematurely, governments save money on pensions and long-term care.
Voters are right to care very much about the health of young people, and to feel that adults have to protect youth from dangerous activities. Humans are hard-wired to be more concerned about novel risks than about familiar ones. The known risks of smoking are accepted, while the novel but lesser risks of vaping are a cause for alarm. The media and many public health agencies are complicit in exaggerating the risk of teen vaping, with talk of an “epidemic” that is undoing years of work on tobacco control, when in fact teen cigarette smoking is down to under 2% and teen vaping has declined rapidly to under 10% in the USA. Parents are horrified by false reports of deaths from “EVALI” and “popcorn lung”, neither of which are caused by legal nicotine vaping. The word “epidemic’ refers to an outbreak of a disease. The inaccurate use of the phrase “vaping epidemic” by medical organizations is unacceptable and must stop.
Every day we continue with only traditional methods of tobacco control, 20,000 smokers around the world die. The plight of 4.2 million Canadian smokers is entirely disregarded because of exaggerated or even false concerns about teenagers. While every effort should be made to educate youth about the addictive nature of nicotine and the health impacts of both vaping and smoking, this should not be allowed to reduce access to current smokers.
Physicians, public health experts and governments tell smokers “Do not vape, we do not know the long-term health effects of vaping”. But when anti-vaxxers say that we do not know the long-term risks of the Covid vaccine, they say: “You should take the vaccine. It is safe. We know what is in it, and we know how people have responded in the past to similar medications. We also know that if people do not take the vaccine, millions will die”. Why are these two issues treated so differently?
Governments that support tobacco harm reduction and less harmful nicotine products
UK
The PSFC document dismisses out-of-hand “reports from the United Kingdom”. This is an important omission, as the UK has the second lowest smoking rates in Europe, and has the least tobacco involvement in public policy. There are two million vapers in the UK who were smokers and have now completely stopped smoking. In the UK only 4% of vapers have never smoked, compared to 38% in Canada. Perhaps there are lessons Canada can learn from a country that sell vapes in main street pharmacies, opens vape shops in hospitals and plans to make e-cigarettes available by prescription. UK Stop Smoking Services report that up to 68% of their clients were able to quit using by vaping. (Vaping in England: an evidence update including vaping for smoking cessation, February 2021)
Sweden
Sweden is a pioneer in tobacco harm reduction and now has the lowest smoking rate in Europe. Over 30 years ago, it introduced snus, an oral tobacco product that users put in their mouth.
“Snus has contributed to decreasing initiation of smoking rather than serving as a gateway to smoking. Smokers who have taken up snus use have quit smoking to a significantly greater extent than smokers without snus use, and a substantial proportion has eventually quit snus use as well and become tobacco-free. These effects have been consistent across five decades. Dual use appears to be a transient state that serves as a stepping-stone to cessation. Snus is the most commonly used self-treatment aid for smoking cessation. Snus has been a major factor behind Sweden’s record-low prevalence of smoking.” – “Patterns of smoking and snus use in Sweden”.
“Sweden boasts Europe’s lowest male lung-cancer death rate — as well as the lowest male death rate from smoking-related cardiovascular diseases, and the lowest male death rate from other cancers that are attributable to tobacco.” It also has the lowest rates of oral and pancreatic cancers in Europe.
More information: Snus – the oral tobacco product that reduced Sweden’s smoking and cancer rates
Japan
Japan has effectively banned vaping, but they have permitted the use of tobacco-containing “Heat-Not-Burn” (HNB) devices, such as iQOS.
HNB devices use a small sachet of tobacco that is warmed to release a vapour that the user inhales. The tobacco is never heated enough for it to burn, so the thousands of toxic chemicals produced by burning tobacco leaves are either absent or present in much lower concentrations than in cigarettes.
In the USA, the Food and Drug Administration (FDA) has authorized the marketing of iQOS as a modified risk tobacco product (MRTP), which permits the marketing of a product that is expected to benefit the health of the population.
Heat not burn devices displaced about 20% of the Japanese cigarette market by 2020. This led to a 43% reduction in cigarette smoking in Japan. By 2021 sales of cigarettes in Japan had fallen by 74 billion cigarettes per year.
More information: Heat-not-burn products lead to a 43% reduction in cigarette smoking in Japan

New Zealand
New Zealand set a smoking prevalence goal of 5% by 2025. “End Smoking New Zealand” and “ASH New Zealand” jointly published “A Surge Strategy”, recommending the use of vaping and other less harmful nicotine products to help achieve that goal.
In April 2021, the NZ Ministry of Health released a regulatory impact statement entitled “Supporting smokers to switch to significantly less harmful alternatives”.
The NZ Ministry of Health established the youth-orientated “QuitStrong.nz” website in August 2020. Quit Strong is one of the first public health initiatives to encourage smokers to use vaping to provide nicotine while maintaining the behavioural and social rituals associated with smoking. The site encourages people to sign on with a Quit Coach who can support them as they switch to vaping.

ASH New Zealand reports that “Vaping is helping Aotearoa New Zealand reach Smokefree 2025. E-cigarette use (vaping) continues to be highly disruptive to smoked cigarettes and presents a fraction of the harm. Creating an environment where smokers can use this much less harmful alternative to manage nicotine addiction is likely to have a significant impact on chronic disease prevention in New Zealand, especially for Maori, Pacific and low-income populations.”
More information: New Zealand has established a vaping strategy that Health Canada should follow.
Conclusions
There are many paths that Canada can follow in an attempt to achieve the goal of a smoking prevalence of 5% by 2035. Following the established tobacco control pathways that have been around for decades with limited success will not achieve our goal.
The examples of snus in Sweden and HNB devices in Japan clearly demonstrates that cigarette smoking can be dramatically reduced by the use of less harmful nicotine products as a substitute for combustible tobacco.
However, given the widespread availability of vaping products in Canada, we should probably look to New Zealand, a country that is on track to achieve its goal of reducing the prevalence of smoking to 5% by 2025, as a source of guidance and inspiration.
Part 7: What should Canadians be told about vaping?
Dr. John Oyston
PSFC has said that Health Canada needs to update its messaging about vaping. This is true. Health Canada has been remiss in not updating its messaging about vaping, and they recognize this. During a December 2021 webinar “Health Canada acknowledged that further public education is needed so that Canadians who smoke are aware that, while vaping is not harmless, it is less harmful than smoking cigarettes for those who quit smoking and completely switch to vaping.”
The mainstream media frequently promote the view that vaping is a ploy by the tobacco industry to lure more young people into tobacco use. They exaggerate its dangers and down-play its benefits. The CBC’s “Vape Fail” series is a notable example of this issue.

In the absence of a clear message from Health Canada, only 4% of Canadians are aware that vaping is much less harmful than smoking. More people think that vaping is worse than smoking than think that it is better. If people who smoke are not aware that vaping is a safer alternative, they will have no motivation to switch.
Unfortunately, not only has Health Canada failed to inform smokers of the health benefits of switching to vaping, but it has also gagged vape shop owners and staff, who are often ex-smokers who understand that switching to vaping saved their lives. They are unable to tell their customers the medical facts about vaping because of Section 30.43 of the Tobacco and Vaping Products Act (TVPA). This prohibits “the promotion of a vaping product in a manner that could cause a person to believe that health benefits may be derived from the use of the product.”
It is not in anyone’s interests for people to make false claims about the benefits of vaping such as “vaping cures cancer!”, but it IS important for smokers to know that scientists have estimated that the risk of getting cancer from vaping is less than 0.5% of the risk of getting cancer from smoking.
In order to resolve this situation, and to clarify what could be said about vaping, Health Canada proposed a “List of Statements for Use in the Promotion of Vaping Products”. This proposal has been put on the back-burner, languishing in Health Canada’s bureaucracy, since September 2018.
HEALTH CANADA’S POTENTIAL STATEMENTS ABOUT VAPING
“List of Statements for Use in the Promotion of Vaping Products”, September 2018.
If you are a smoker, switching completely to vaping is a much less harmful option
While vaping products emit toxic substances, the amount is significantly lower than in tobacco smoke
By switching completely to vaping products, smokers are exposed to a small fraction of the 7,000 chemicals found in tobacco smoke
Switching completely from combustible tobacco cigarettes to e-cigarettes significantly reduces users’ exposure to numerous toxic and cancer-causing substances
Completely replacing your cigarette with a vaping product will significantly reduce your exposure to numerous toxic and cancer causing substances
Switching completely from smoking to e-cigarettes will reduce harms to your health
Since then, other groups have made additional suggestions.
ADDITIONAL STATEMENTS ABOUT VAPING
The Electronic Cigarette Trade Association of Canada suggested some minor changes to the Health Canada wording and proposed adding:
Second hand vapour represents a small fraction of risk compared to second hand smoke
Vaping is typically far less expensive than smoking
Tobacco smoke often has a strong, unpleasant odour when compared to vapour
New Zealand Ministry of Health & NZ Health Promotion Agency “Vaping Facts” website, June 2019.
Vaping has the potential to help people quit smoking and contribute to New Zealand’s Smokefree 2025 goal
Nicotine is addictive, but it’s the toxins produced by burning tobacco that cause smoking-related illnesses
Vaping can vary from no nicotine to high nicotine, and is much less harmful than smoking
Vaping has helped many people quit smoking and is a legitimate way to become smoke-free
Breathing any product into your lungs unnecessarily is not ideal, and that’s why non-smokers should not vape. However, for those who smoke, switching to vaping is likely to substantially reduce health risks.
The Centre for Addiction and Mental Health, (CAMH) “Lower-Risk Nicotine Use Guidelines” based on a review of the literature up to October 2019.
Make the switch to nicotine products that do not burn.
Further reduce your risk by switching to products that don’t have tobacco like NRT or e-cigarettes
Do not purchase unsafe illicit/black market e-liquids, pods or devices
Don’t adulterate your products (THC, vitamin E, other oils, etc.) or modify the device
Keep the products away from children
Receive instruction on the use of the device given the variability in device types
E-cigarettes as a cessation aid may be most effective when combined with behavioural counselling
Smokers should be advised to switch completely from combustible tobacco to e-cigarettes and to use e-cigarettes when they would normally have smoked
Continued use of e-cigarettes may reduce risk of relapse to combustible tobacco
Vape shops should be allowed and encouraged to use these statements when talking about vaping.
Physicians for a Smoke-Free Canada proposed messages
PSFC has also proposed that Health Canada should change its messaging about vaping.
“A more truthful, blunter message to young people is warranted. Something like: Smoking kills, and vaping almost certainly kills too.”
This ridiculous statement belongs with “Reefer Madness” as a bizarre example of exaggerating risk to an implausible level. Health Canada reports that 48,000 Canadians die from smoking every year, and “acknowledged that there have been no deaths reported as a result of vaping-related illnesses in Canada.”
In the UK over a five year period there were three deaths reported as possibly being associated with vaping in a population of 2.7 million adult vapers. In the same period of time 390,00 people died from smoking.
PSFC also recommended that Health Canada should advise smokers that:
“Using e-cigarettes will likely decrease the chances of success but will increase health risks in comparison with approved smoking cessation aids.”
This topic was reviewed in Part 4.
The data was also summarized in “Vaping in England: an evidence update including vaping for smoking cessation, February 2021” “Three systematic reviews consistently found vaping products containing nicotine were significantly more effective for helping people stop smoking than NRT. This finding was supported by two non-randomised studies that reported higher quit rates of people using a vaping product who attended a stop smoking service, compared with those who used NRT.”
Recommendations
Health Canada should work with their counterparts in the UK and New Zealand in recognizing and supporting vaping as both a critical addition to our smoking cessation armamentarium and as a form of harm reduction for smokers who are dependent on nicotine. It needs to convey that message to the public clearly through its website, through public service announcements and on informational inserts in cigarette packages.
The Canadian government should immediately repeal Section 30.43 of the Tobacco and Vaping Products Act, removing the gag order on vape shops. The vaping industry should be on an equal footing with other businesses, and have the same penalties for false advertising as any other consumer product. Vape shop staff should be trained, encouraged, and funded to educate smokers about the benefits of completely switching to vaping.
These matters are urgent. About four thousand Canadians die every month from tobacco use. We know that if we can persuade adults to stop smoking, we can prevent most of the disease, disability and death caused by tobacco.
They need to be told that, if they cannot quit using nicotine because of withdrawal symptoms and cravings, there are a range of less harmful sources of nicotine available to them, including vaping. It is Health Canada’s responsibility to spread this information, as part of its mandate to help Canadians maintain and improve their health and reduce risks. Canada’s vape stores should be allowed to be active participants and partners in that process.
WHO WE ARE
This report was commissioned and paid for by the Canadian Vaping Association (CVA). There are some people who would stop reading and trash this report as tobacco industry lies as soon as they find that out. Please take a moment to find out about the CVA and the three doctors who wrote this report first.
The CVA’s long term vision is a smoke-free Canada achieved through consumer awareness of the relative risk of vaping and balanced regulation. The CVA remains committed to working with various levels of government and regional health authorities to implement regulations which balance access for adult smokers with youth protection. The CVA has no affiliation to the tobacco industry.
We are three doctors (two medical, and one PhD). We have come together from different backgrounds to write this because we want to reduce the disease, disability and death caused by tobacco smoking. We believe that Canada’s 4.2 million smokers deserve accurate information about the comparative risks of different sources of nicotine that are available to them so that they have the autonomy to make their own health choices.
Dr. John Oyston MB BS, BMedSci, FRCA, FRCP(C) spent forty years working as an anesthesiologist. He cared for people who acquired diseases by smoking that led to cancer surgery or amputations. This made him a tobacco control activist. He founded “Stop Smoking for Safer Surgery”, supported the Tobacco 21 movement, and is now a strong supporter of vaping as a way to quit smoking, and as a safer alternative for smokers who are dependent on nicotine.
You can find his blog posts on topics such as Tobacco Harm Reduction, watch a five minute video he contributed to Global Forum on Nicotine and find his list of publications at PubMed. His email address is [email protected] .
Dr. Chris Lalonde PhD is a professor of psychology at the University of Victoria. His research interests include identity development and social development in childhood and adolescence. He has worked extensively on issues of youth health and wellbeing with First Nations communities in British Columbia and Manitoba. This work focuses on the relation between local efforts to pursue self-government and promote traditional practices and culture and the effects of provincial and federal policies on the lived experience of youth. He has personal experience of quitting smoking by vaping.
You can read his op-ed “Governments must find optimal regulatory balance with vaping”, watch his video about youth vaping on Regulator Watch, and study his list of publications on Google Scholar. His email address is [email protected] .
Dr. Mark Tyndall MD, ScD, FRCPC has focused his medical and public health career on working with populations at risk. His work with people who use drugs began in 1995 and he has made important contributions to a range of harm reduction innovations including needle distribution, supervised injection sites and safer drug supply programs. Mark’s introduction to vaping came in 2012 when he realized that his clinical HIV practice was dominated by illnesses and deaths that were primarily related to cigarettes and that nothing was being done about it. A strong proponent of evidence-based public health policy and interventions, Mark has authored over 300 academic papers and has received multiple honours for his work.
He gave a Ted Talk on “The harm reduction model of drug addiction treatment”, which has had over 1.4 million views. He presented at the 2021 Global Forum on Nicotine. You can find a list of his publications on Google Scholar. His email address is [email protected] .
It can be very hard to separate truth from lies about vaping. Organizations that should be trustworthy, such as the Center for Disease Control and the American Lung Association have lied about vaping. We ask that you trust us because we have decades of history in caring for our patients. We are working together because we believe that vaping and other forms of tobacco harm reduction are the only logical way forward to significantly decrease tobacco deaths and meet the goal of eliminating smoking. Most often we study, write, speak and teach for free, but sometimes we take unrestricted grants from the tobacco and vaping industry when this provides resources to devote to our passion and gives us a platform to speak to more people and to spread our message more widely.
SUMMARY
Rebuttal Of The PSFC Report
1) Vaping experimentation by young people has decreased from a peak of 22.4% to under 10% in the USA, and seems to have peaked in Canada as well.
2) Teen smoking rates are one sixth of what they were 40 years ago. Vaping is a diversion from smoking, rather than a gateway to smoking.
3) Dual use is often part of the transition to vaping. Everyone trying to quit smoking will go through a transition phase, but the sooner they completely stop smoking, the better.
4) Vaping is both a much safer alternative source of nicotine for people who have become dependent on nicotine through smoking, and an effective way to quit. Like all other methods of quitting, it is more successful when done with support and accurate information.
5) Vaping can have unwanted side effects, just like any other treatment. People who would not benefit should not start vaping. The long-term health risks are unlikely to be more than a small fraction of the health risks from smoking. Smokers who switch to vaping benefit from both subjective and objective improvements in their health.
6) Other countries, such as Sweden and Japan, are benefiting from smokers switching to less harmful nicotine products. Health Canada should look to New Zealand and the UK for a strategy to use vaping to assist in achieving its “Tobacco Endgame” goals.
7) It is essential that Canada’s 4.2 million smokers are given accurate information about less harmful forms of nicotine and not misled with false information about “EVALI” and “popcorn lung”.
Further Recommendations
Health Canada should recognize the benefits of vaping as an essential additional smoking cessation tool that can help it reach its “Tobacco Endgame” goal of a 5% smoking prevalence by 2035. Vaping may be especially effective in specific groups such as indigenous peoples and people living with mental illness, where smoking prevalence remains high and conventional treatments have failed. Health Canada should fund research into optimizing vaping as a way to quit, to measure the health effects of switching, and to monitor the long-term health impact of vaping.
There is no “wrong way” to quit smoking. Whether smokers go to their family doctor, a “Stop Smoking” clinic, a pharmacist or a vape shop they should get accurate information about all their options, including vaping. Vape store staff should be allowed to discuss the health benefits of switching to vaping. Vaping equipment should be sold wherever cigarettes are sold. It should also be available in pharmacies and on prescription where it can be covered by health insurance programs. Vaping should be incorporated into anti-smoking campaigns and smoking cessation programs such as the “Smokers’ Quitline”.